Enhancing Smoking Cessation in the Homeless Population The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Smoking Cessation in Homeless Populations: A Pilot Clinical Trial Kolawole S. Okuyemi, M.D., M.P.H. Program in Health Disparities Research, Department of Family Medicine and Community Health, University of Minnesota Medical School.
Abstract
Introduction:Although homeless individuals smoke at an alarmingly high rate, few smoking cessation clinical trials have focused on this vulnerable population. Little is known about recruitment efforts and suitable eligibility criteria for tobacco control research in homeless populations.Methods:The aim of this article is to describe the recruitment, eligibility, and enrollment of homeless smokers who participated in the Power to Quit smoking study, a randomized smoking cessation clinical trial funded by the National Institutes of Health. The study compared motivational interviewing and standard counseling while participants received an 8-week treatment of the nicotine patch.Results:Working with local emergency shelters, a total of 839 adult smokers were screened for study eligibility, 580 of whom (69.1%) met eligibility criteria. Of those eligible, 430 (74.1%) returned for randomization. Those who returned for randomization were older and more likely to have a phone number compared with eligible participants not enrolled. The most common reasons for exclusion included exhaled carbon monoxide levels less than or equal to 5 parts per million (indicating nonsmoking status), use of smoking cessation aid during the past 30 days, and not meeting the study definition of homelessness.Conclusion:Knowledge of these factors may help researchers tailor criteria that accurately identify and include homeless smokers in future research.
Journal
Nicotine and Tobacco Research – Oxford University Press
Smoking Cessation In Homeless Populations A Pilot Clinical Trial 2017
Published: Mar 24, 2014
Smoking Cessation In Homeless Populations A Pilot Clinical Trials
Background Although smoking prevalence remains strikingly high in homeless populations (~70% and three times the US national average), smoking cessation studies usually exclude homeless persons. Novel evidence-based interventions are needed for this high-risk subpopulation of smokers.
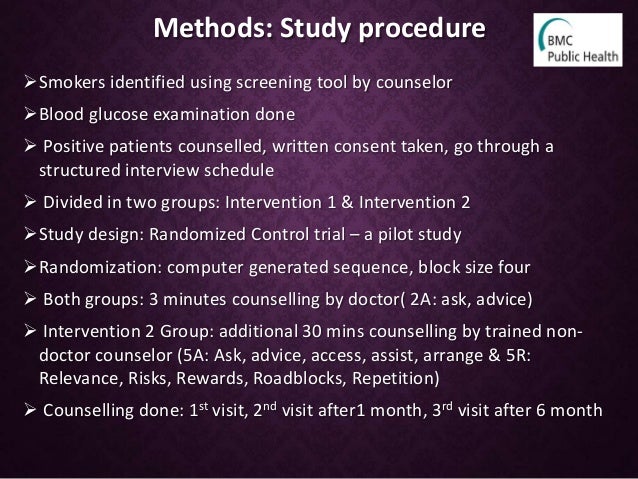
Purpose To describe the aims and design of a first-ever smoking cessation clinical trial in the homeless population. The study was a two-group randomized community-based trial that enrolled participants (n = 430) residing across eight homeless shelters and transitional housing units in Minnesota. The study objective was to test the efficacy of motivational interviewing (MI) for enhancing adherence to nicotine replacement therapy (NRT; nicotine patch) and smoking cessation outcomes.
Smoking Cessation In Homeless Populations A Pilot Clinical Trial 2016
Methods Participants were randomized to one of the two groups: active (8 weeks of NRT + 6 sessions of MI) or control (NRT + standard care). Participants attended six in-person assessment sessions and eight retention visits at a location of their choice over 6 months. Nicotine patch in 2-week doses was administered at four visits over the first 8 weeks of the 26-week trial. The primary outcome was cotinine-verified 7-day point-prevalence abstinence at 6 months. Secondary outcomes included adherence to nicotine patch assessed through direct observation and patch counts. Other outcomes included the mediating and/or moderating effects of comorbid psychiatric and substance abuse disorders.
Results Lessons learned from the community-based cessation randomized trial for improving recruitment and retention in a mobile and vulnerable population included: (1) the importance of engaging the perspectives of shelter leadership by forming and convening a Community Advisory Board; (2) locating the study at the shelters for more visibility and easier access for participants; (3) minimizing exclusion criteria to allow enrollment of participants with stable psychiatric comorbid conditions; (4) delaying the baseline visit from the eligibility visit by a week to protect against attrition; and (5) regular and persistent calls to remind participants of upcoming appointments using cell phones and shelter-specific channels of communication.
Limitations The study’s limitations include generalizability due to the sample drawn from a single Midwestern city in the United States. Since inclusion criteria encompassed willingness to use NRT patch, all participants were motivated and were ready to quit smoking at the time of enrollment in the study. Findings from the self-select group will be generalizable only to those motivated and ready to quit smoking. High incentives may limit the degree to which the intervention is replicable.
Conclusions Lessons learned reflect the need to engage communities in the design and implementation of community-based clinical trials with vulnerable populations.
| 1. | Mokdad, A, Marks, J, Stroup, D, Gerberding, J. Actual causes of death in the United States, 2000. JAMA 2004; 291(10): 1238–45. Google Scholar | Crossref | Medline | ISI |
| 2. | The United States Conference of Mayors . Hunger and Homelessness Survey: A Status Report on Hunger and Homelessness in America’s Cities. A 27-City Survey. December2009. Google Scholar |
| 3. | Wilder Research Center . Homelessness in Minnesota 2009: Results of the Wilder Statewide Survey. Wilder Research, St. Paul, Minnesota, 2010. Google Scholar |
| 4. | Wilder Research Center . Homelessness in Minnesota 2003: Key Facts from the Survey of Minnesotans without Permanent Housing. Amherst H. Wilder Foundation, St. Paul, MN, 2004. Google Scholar |
| 5. | Baggett, TP, Rigotti, NA. Cigarette smoking and advice to quit in a national sample of homeless adults. Am J Prev Med 2010; 39(2): 164–72. Google Scholar | Crossref | Medline | ISI |
| 6. | Kushel, MB, Miaskowski, C. End-of-life care for homeless patients: ‘She says she is there to help me in any situation’. JAMA 2006; 296(24): 2959–66. Google Scholar | Crossref | Medline | ISI |
| 7. | Song, J, Ratner, ER, Bartels, DM. Experiences with and attitudes toward death and dying among homeless persons. J Gen Intern Med 2007; 22(4): 427–34. Google Scholar | Crossref | Medline | ISI |
| 8. | Kung, H-C, Hoyert, D, Xu, J, Murphy, SL. Deaths: Final data for 2005. National Vital Statistics Report 2008; 56(10). Google Scholar | Medline |
| 9. | Hwang, SW . Mortality among men using homeless shelters in Toronto, Ontario. JAMA 2000; 283(16): 2152–57. Google Scholar | Crossref | Medline | ISI |
| 10. | Hwang, SW, Orav, EJ, O’Connell, JJ, Lebow, JM, Brennan, TA. Causes of death in homeless adults in Boston. Ann Intern Med 1997; 126(8): 625–28. Google Scholar | Crossref | Medline | ISI |
| 11. | Morrison, DS . Homelessness as an independent risk factor for mortality: Results from a retrospective cohort study. Int J Epidemiol 2009; 38(3): 877–83. Google Scholar | Crossref | Medline | ISI |
| 12. | Gelberg, L, Gallagher, TC, Andersen, RM, Koegel, P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Pub Health 1997; 87(2): 217–20. Google Scholar | Crossref | Medline | ISI |
| 13. | Gelberg, L, Andersen, RM, Leake, BD. The behavioral model for vulnerable populations: Application to medical care use and outcomes for homeless people. Health Serv Res 2000; 34(6): 1273–302. Google Scholar | Medline | ISI |
| 14. | Teeter, T . Adherence: Working with homeless populations. Focus 1999; 14(2): 5–6. Google Scholar | Medline |
| 15. | Okuyemi, K, Caldwell, A, Thomas, J. Homelessness and smoking cessation: Insights from focus groups. Nicotine Tob Res 2006; 8(2): 287–96. Google Scholar | Crossref | Medline | ISI |
| 16. | Arnsten, JH, Reid, K, Bierer, M, Rigotti, N. Smoking behavior and interest in quitting among homeless smokers. Addict Behav 2004; 29(6): 1155–61. Google Scholar | Crossref | Medline | ISI |
| 17. | Connor, S, Cook, R, Herbert, M, Neal, S, Williams, J. Smoking cessation in a homeless population: There is a will, but is there a way? J Gen Intern Med 2002; 17(5): 369–72. Google Scholar | Medline | ISI |
| 18. | Okuyemi, KS, Thomas, JL, Hall, S. Smoking cessation in homeless populations: A pilot clinical trial. Nicotine Tob Res 2006; 8(5): 689–99. Google Scholar | Crossref | Medline | ISI |
| 19. | Shelley, D, Cantrell, J, Warn, D, Wong, S. Smoking cessation among sheltered homeless: A pilot. Am J Health Behav 2010; 34(5): 544–52. Google Scholar | Crossref | Medline | ISI |
| 20. | Miller, WR, Rollnick, S. Motivational Interviewing: Preparing People to Change. Guildford Press, New York, 2002. Google Scholar |
| 21. | Butler, C, Rollnick, S, Cohen, D. Motivational consulting versus brief advice for smokers in general practice: A randomised trial. Br J Gen Pract 1999; 49: 611–16. Google Scholar | ISI |
| 22. | Colby, SM, Monti, PM, Barnett, NP. Brief motivational interviewing in a hospital setting for adolescent smoking: A preliminary study. J Consult Clin Psychol 1998; 66(3): 574–78. Google Scholar | Crossref | Medline | ISI |
| 23. | Heckman, CJ, Egleston, BL, Hofmann, MT. Efficacy of motivational interviewing for smoking cessation: A systematic review and meta-analysis. Tob Control 2010; 19(5): 410–16. Google Scholar | Crossref | Medline | ISI |
| 24. | Slama, K, Redman, S, Perkins, J, Reid, A, Sanson-Fisher, RW. The effectiveness of two smoking cessation programs for use in general practice: A randomized clinical trial. BMJ 1990; 300: 1707–09. Google Scholar | Crossref | Medline |
| 25. | A clinical practice guideline for treating tobacco use and dependence: A US Public Health Service report . The Tobacco Use and Dependence Clinical Practice Guideline Panel, Staff, and Consortium Representatives. JAMA 2000; 283(24): 3244–54. Google Scholar | Crossref | Medline |
| 26. | US Code . Title 42, Chapter 119, Subchapter I, Section 11302. 2004. Available at http:/www4.law.cornell.edu/usdoce/42/11302.html (accessed 26 September 2011). Google Scholar |
| 27. | Middleton, ET, Morice, AH. Breath carbon monoxide as an indication of smoking habit. Chest 2000; 117(3): 758–63. Google Scholar | Crossref | Medline | ISI |
| 28. | Society for Research on Nicotine and Tobacco (SRNT) . Biochemical verification of tobacco use and cessation. Nicotine Tob Res 2002; 4(2): 149–59. Google Scholar | Crossref | Medline |
| 29. | Tonnesen, P, Norregaard, J, Mikkelsen, K, Jorgensen, S, Nilsson, F. A double-blind trial of a nicotine inhaler for smoking cessation. JAMA 1993; 269(10): 1268–71. Google Scholar | Crossref | Medline | ISI |
| 30. | Sheehan, DV, Lecrubier, Y, Sheehan, KH. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59(Suppl. 20): 22–33, quiz 34–57. Google Scholar | Medline | ISI |
| 31. | Butler, J, Okuyemi, KS, Jean, S. Smoking characteristics of a homeless population. Subst Abus 2002; 23(4): 223–31. Google Scholar | Crossref | Medline |
| 32. | Okuyemi, KS, Caldwell, AR, Thomas, JL. Homelessness and smoking cessation: Insights from focus groups. Nicotine Tob Res 2006; 8(2): 287–96. Google Scholar | Crossref | Medline | ISI |
| 33. | Morisky, DE, Green, LW, Levine, DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986; 24(1): 67–74. Google Scholar | Crossref | Medline | ISI |
| 34. | Everson, SA, Goldberg, DE, Kaplan, GA. Hopelessness and risk of mortality and incidence of myocardial infarction and cancer. Psychosom Med 1996; 58(2): 113–21. Google Scholar | Crossref | Medline | ISI |
| 35. | Everson, SA, Kaplan, GA, Goldberg, DE, Salonen, JT. Hypertension incidence is predicted by high levels of hopelessness in Finnish men. Hypertension 2000; 35(2): 561–67. Google Scholar | Crossref | Medline | ISI |
| 36. | Etter, JF, Bergman, MM, Humair, JP, Perneger, TV. Development and validation of a scale measuring self-efficacy of current and former smokers. Addiction 2000; 95(6): 901–13. Google Scholar | Crossref | Medline | ISI |
| 37. | Williams, GC, Cox, EM, Kouides, R, Deci, EL. Presenting the facts about smoking to adolescents: Effects of an autonomy-supportive style. Arch Pediatr Adolesc Med 1999; 153(9): 959–64. Google Scholar | Crossref | Medline |
| 38. | Cox, LS, Tiffany, ST, Christen, AG. Evaluation of the brief questionnaire of smoking urges (QSU-brief) in laboratory and clinical settings. Nicotine Tob Res 2001; 3(1): 7–16. Google Scholar | Crossref | Medline |
| 39. | Rost, K, Burnam, MA, Smith, GR. Development of screeners for depressive disorders and substance disorder history. Med Care 1993; 31(3): 189–200. Google Scholar | Crossref | Medline | ISI |
| 40. | Kroenke, K, Spitzer, RL. The PHQ-9: A new diagnostic and severity measure. Psychiatr Ann 2002; 32(9): 509–15. Google Scholar | Crossref | ISI |
| 41. | Cohen, S, Kamarck, T, Mermelstein, R. A global measure of perceived stress. J Health Soc Behav 1983; 24(4): 385–96. Google Scholar | Crossref | Medline | ISI |
| 42. | Volmink, J, Matchaba, P, Garner, P. Directly observed therapy and treatment adherence. Lancet 2000; 355(4): 1345–49. Google Scholar | Crossref | Medline | ISI |